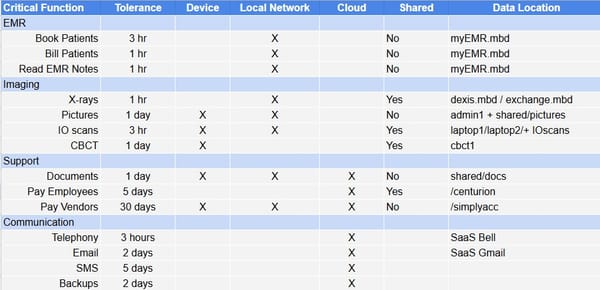
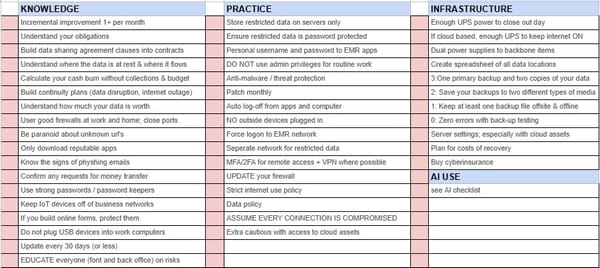
Deep Dive: Monitoring Large Leukoplakia - Weighing the Utility of Adjunctive Techniques in Clinical Practice
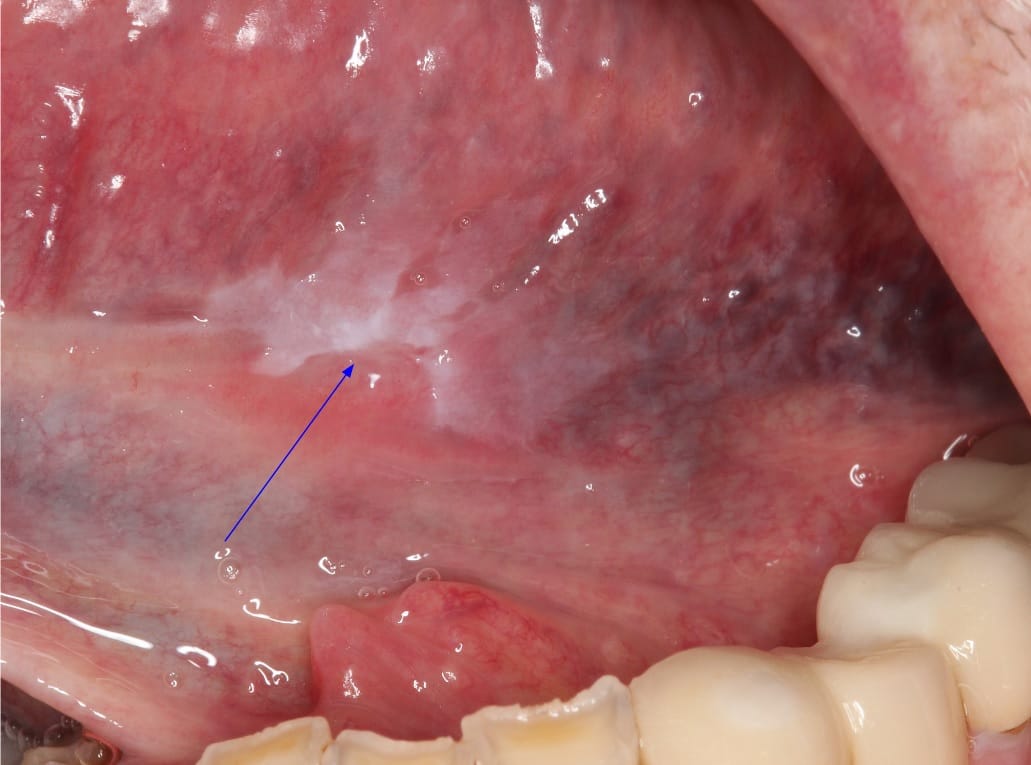
I was recently dealing with an extensive leukoplakic lesion, where complete removal wasn’t feasible, and the monitoring approach shifts from immediate treatment to careful, ongoing assessment. I'm adding this deep dive to look at a variety of adjunctive techniques that have gained traction in recent years, from light-based detection systems to brush biopsy, and even immunohistochemical testing like Stratocyte. Yet, the question remains: do these methods add meaningful value beyond the traditional visual examination and biopsy? See my previous post on malignant transformation to determine the risk of cancer.
Clinical Follow-Up as a Foundation
Regular clinical follow-up is essential in managing oral potentially malignant disorders (OPMDs), with evidence suggesting that structured follow-up can improve outcomes through early intervention. Visual examination is still the primary tool for ongoing assessment, particularly for practitioners without immediate access to advanced diagnostic technology. While not definitive on its own, visual examination remains a valuable baseline method, enabling clinicians to spot any obvious changes in lesion size, color, or texture. In addition, repeat photographs to better find changes under white light can be important.
Adjunctive Techniques: Enhancing or Complicating?
Adjunctive techniques are increasingly available, marketed as tools that can augment the visual examination. However, their role in managing established leukoplakia is nuanced. Here’s how some of these methods are currently positioned in the field:
Light-Based Detection Systems
Several light-based detection systems use specific wavelengths of light, sometimes combined with photosensitizing agents, to highlight potential areas of concern. Devices such as VELscope, Vizilite Plus, and Identafi are frequently mentioned. The goal is to improve visualization, particularly of submucosal changes that might not be apparent under white light.
However, it’s worth noting that these systems have limitations. Studies to date have yet to demonstrate that light-based detection provides a significant advantage over standard biopsy in terms of sensitivity or specificity for monitoring leukoplakia. In my experience, while blue or white light techniques can occasionally help direct attention to certain areas, they do not replace biopsy for accurate histopathological assessment.
Brush Biopsy and Computer Analysis
Brush biopsy is a minimally invasive technique that collects cells from the lesion surface for cytological analysis, often aided by computer algorithms. While brush biopsy can identify areas with cellular abnormalities, it doesn’t provide the depth of information available through a traditional biopsy. In my experience, its diagnostic value remains limited for larger lesions that require a full histological workup.
Biopsy: Still the Benchmark for Monitoring
In terms of accuracy, biopsy and subsequent histopathological examination remain the most reliable approach for assessing leukoplakia. This is particularly true in non-homogeneous lesions where areas of dysplasia may vary. In these cases, experienced clinicians often select biopsy sites based on clinical characteristics, sometimes aided by adjunctive methods like toluidine blue, to highlight high-risk areas.
Histopathological examination provides not only confirmation of the diagnosis but also grading of dysplasia, which guides management decisions. Repeat biopsies where clinical changes are observed over time, is my usual tactic to monitor pathologic changes over time.
Immunohistochemical Testing: Stratocyte and Emerging Biomarkers
Recently, immunohistochemical testing has been explored as a way to gain additional insight into the molecular profile of leukoplakia lesions. Stratocyte, for example, offers a biomarker analysis intended to identify dysplastic changes at the molecular level, potentially distinguishing higher-risk leukoplakia from lesions with lower malignant potential.
While promising, immunohistochemical testing remains an adjunctive tool rather than a standalone solution. Stratocyte and similar tests could, in theory, refine risk stratification, but their integration into routine practice is still emerging. For most clinicians, these tests may complement histopathology by adding a molecular layer of assessment, though they should not be seen as a replacement for a traditional biopsy.
Conclusion: A Balanced Approach to Monitoring
In summary, adjunctive techniques like white light photography, blue light, and immunohistochemical testing provide potential supplementary information but are best used alongside, rather than in place of, biopsy and histopathology. In large or intractable leukoplakia, biopsy remains the gold standard for monitoring, with adjuncts adding potential insight without superseding the value of a comprehensive histopathological assessment.