Deep Dive: Updated Guidelines on Implant Placement and Medication-Related Osteonecrosis of the Jaw (MRONJ)

As an oral surgeon, I’m seeing more patients than ever on antiresorptive medications, primarily for osteoporosis or cancer-related bone conditions. In Canada alone, over 2 million people are affected by osteoporosis, with many receiving bone-sparing therapies such as bisphosphonates and denosumab (CMAJ). This prevalence underscores the importance of understanding how these therapies impact dental procedures, particularly implant placement. To address these considerations, the American Association of Oral and Maxillofacial Surgeons (AAOMS) has recently updated its position paper on medication-related osteonecrosis of the jaw (MRONJ), offering essential insights and guidelines for dental professionals.
For easy access, the full AAOMS Position Paper on MRONJ can be viewed here.
Key Findings Reported
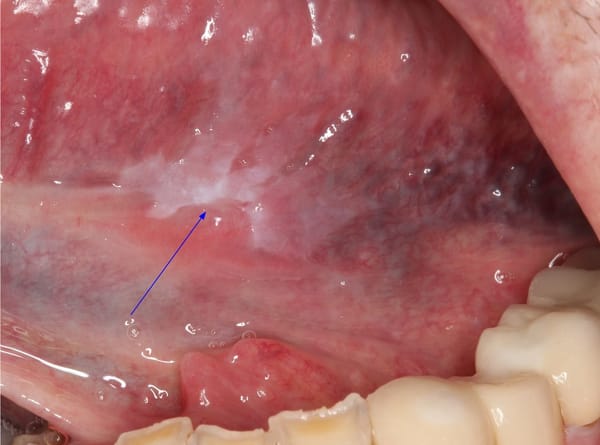
Key findings from the AAOMS report indicate that 75% of MRONJ cases occur in the mandible, highlighting this site as particularly vulnerable in patients undergoing antiresorptive therapy. The report also noted that implants which were well-placed, fully functioning, and free of peri-implantitis did not fail, underscoring the importance of precise implant placement and peri-implant health. The average time to MRONJ onset was reported as 46.5 ± 33.2 months, with patients with osteoporosis experiencing a significantly longer delay to MRONJ onset—about three times longer—compared to patients with cancer. Furthermore, the presence of peri-implantitis was identified as a substantial risk factor for MRONJ development, irrespective of the time elapsed since implant placement, highlighting the necessity for ongoing peri-implantitis management in these patients.
Key Changes and Updated Understanding of MRONJ
The latest AAOMS position paper builds upon prior guidelines (2009 and 2014), integrating findings that deepen our understanding of MRONJ’s pathophysiology and management. Notably, the updated guidelines affirm that MRONJ risk, while generally low, is significantly influenced by medication type, dosage, and cumulative exposure. Here are some crucial points:
- Risk Differentiation by Medication: AAOMS now provides more distinct guidance based on specific medications. For instance, bisphosphonates (BPs), such as alendronate and zoledronic acid, and denosumab (a RANK-L inhibitor), are commonly prescribed for osteoporosis. Both drugs are linked to a risk of MRONJ; however, denosumab demonstrates a shorter duration of action, with effects on bone resorption diminished within approximately six months after discontinuation. This shorter action window provides an opportunity for careful treatment timing in high-risk patients.
- Surgical Interventions: The AAOMS guidelines continue to recommend that elective procedures, such as implant placement, are approached cautiously, especially in oncology patients receiving intravenous antiresorptives, who present a much higher risk of MRONJ compared to osteoporotic patients. Cancer patients receiving antiresorptive therapy face MRONJ rates between 1% and 5% following extractions, a known high-risk procedure, compared to about 0.02% to 0.05% in osteoporotic patients on oral bisphosphonates.
- Drug Holidays and Timing Considerations: The guidelines still note the lack of conclusive evidence supporting the efficacy of drug holidays in MRONJ prevention. However, it may be prudent to pause denosumab administration in patients requiring invasive procedures, as it can potentially reduce MRONJ risk by allowing bone turnover to resume briefly. While this approach remains somewhat controversial, it’s considered reasonable, particularly in patients with moderate to high cumulative medication exposure.
Practical Takeaways for General Dentists
- Patient Assessment and History: A thorough medical and dental history is critical for patients on antiresorptive medications. Ensure close collaboration with the patient's physician to understand their specific medication regimen, cumulative exposure, and overall health risks.
- Non-Surgical Alternatives and Informed Consent: Where possible, consider non-surgical options for high-risk patients. When surgery is necessary, thoroughly discuss the MRONJ risk with patients, especially when their medication history includes prolonged use of antiresorptives.
- Management Strategy: For patients on bisphosphonates, if dental implants are under consideration, shorter-term exposure to oral bisphosphonates generally poses a lower risk. For patients on denosumab or intravenous bisphosphonates, a multidisciplinary approach involving the patient's medical team may help tailor a plan that minimizes risk, potentially utilizing drug holidays as appropriate based on the latest clinical judgment.
This update underscores the importance of preventive care and careful planning for patients on bone-sparing therapies, balancing the need for dental interventions with an awareness of the risks these medications pose for long-term bone healing and implant success.