Deep Dive: Strategic Risk Management for Dental Implant Surgery
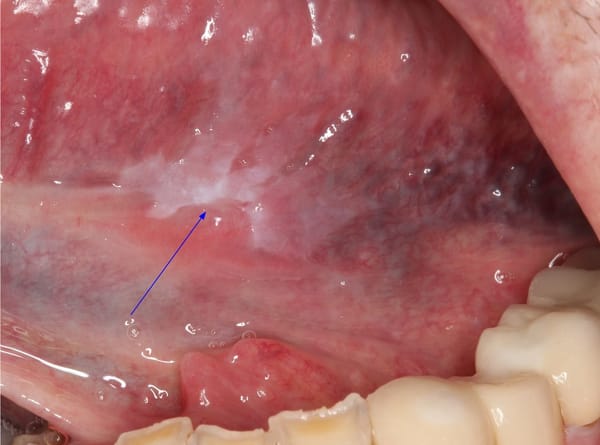
We now better understand the factors associated with implant failure, as well as the potential for unaesthetic or non-functional outcomes and we’ve developed strategies to avoid catastrophic complications.
In the last 20 years, the clinical and scientific community has built a large cache of data on the risks in implant surgery. We now better understand the factors associated with implant failure, as well as the potential for unaesthetic or non-functional outcomes, and we’ve developed strategies to avoid catastrophic complications. Adopting a frontline strategy to use this knowledge systematically, enhancing both patient safety and clinical success, requires rigor. In this series, I’ll dive into specific risks, but I'd like to start with the basics: a risk management framework for dental implant surgery and how I approach risk mitigation.
Understanding Risk in Clinical Practice
In risk management, we define risk as Risk = Threat x Vulnerability. For dental implants, “threats” include common complications like peri-implantitis or improper osseointegration, while “vulnerabilities” are factors that can intensify these risks, such as smoking or compromised bone quality. A well-rounded approach to managing these risks means evaluating each threat-vulnerability interaction in every case. By using a structured assessment process, we make prevention part of our baseline approach rather than an afterthought.
The Role of Mild vs. Wild-Type Risks
In clinical settings, risk generally falls into two categories:
- Mild Risks (Wikipedia): These are lower-impact events that occur frequently enough to be measurable, like mild post-op inflammation or minor discomfort. Because they are so common, we can quantify them, study their patterns, and establish reliable preventative measures.
- Wild-Type Risks (Wikipedia): Wild-type risks are rarer but have potentially high-impact consequences, such as nerve damage or severe infection. They don’t occur often enough to be easily measurable, making them harder to predict. Instead of quantifying wild-type risks, we monitor “close calls”—those incidents that nearly led to significant outcomes but were intercepted. Tracking close calls can reveal patterns that might help us identify ways to preempt these rare events.
In risk management, both categories play a role. Mild risks are managed through protocols and education, while wild-type risks require vigilance and reflection, using close-call analysis to adapt our approach continually.
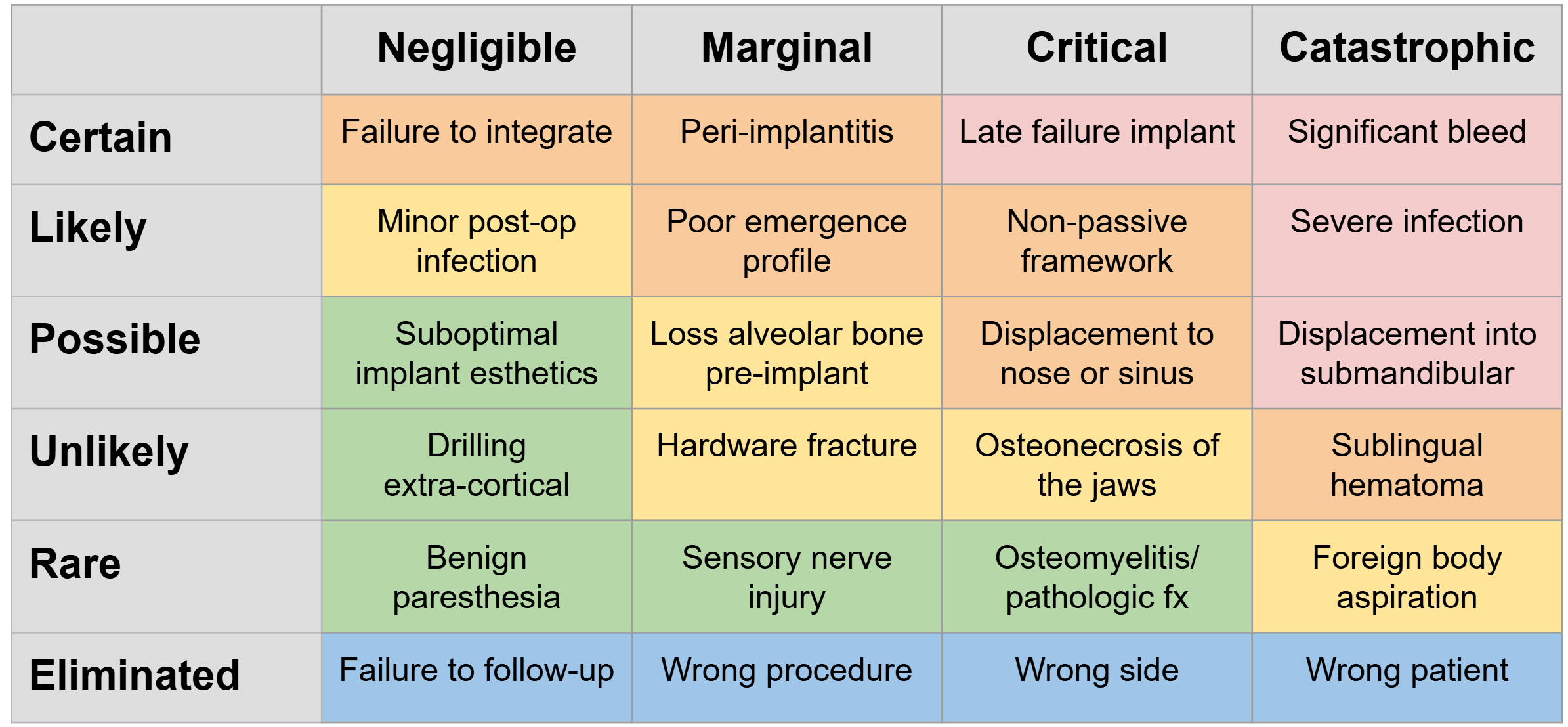
The Risk Management Matrix: Prioritizing Actions
The risk management matrix (Wikipedia) is a valuable tool for organizing risks based on their likelihood and impact. Here’s how it guides decision-making for each patient:
- Low Likelihood, Low Impact (Minor Events): These include issues like temporary swelling or mild sensitivity. For these, it’s usually enough to inform the patient and monitor recovery.
- High Likelihood, Low Impact (Frequent Risks): Common events, like post-op inflammation, call for standardized protocols. Frequent risks can be anticipated and managed predictably.
- Low Likelihood, High Impact (Wild-Type Events): Rare but serious events, like peri-implant osteonecrosis, require monitoring and strategic planning, informed by past close-call experiences.
- High Likelihood, High Impact (Complex Cases): Patients with complex needs, such as compromised bone quality, demand extra precautions and often require detailed patient consent before proceeding.
This matrix approach allows us to make informed decisions that prioritize patient safety without overcomplicating routine cases.
Proactive Patient Assessment: Establishing a Risk Baseline
Effective risk management begins with a comprehensive patient assessment to establish a risk profile. By identifying individual vulnerabilities, we can adapt each treatment plan to reduce the likelihood of both mild and wild-type risks.
Key considerations include:
- Lifestyle Factors: Smoking and medications, for instance, are known to increase the rate of complications.
- Medical History: Conditions like cancer or prior periodontal disease can influence healing and implant stability.
- Anatomical Challenges: Bone quality and nerve positioning play a role in planning for both esthetics and functionality.
An assessment that accounts for these factors doesn’t just improve clinical outcomes; it also builds trust. Patients who understand their personalized risk profile and mitigation plan are more likely to adhere to post-op protocols and attend follow-ups.
Technical Analysis in Risk Management
Technical analysis provides mathematical tools to systematically assess and monitor risks in dental implant surgery:
- Expected Value of Risk (Wikipedia): Expected value helps us evaluate the overall “weight” of a risk by combining its likelihood and severity. For example, mild risks that are highly probable can be given similar attention to low-probability but severe events because their “expected cost” is comparable.
- Decision Trees and Conditional Probability (Wikipedia): Decision trees let us map out treatment pathways and estimate different outcomes based on patient-specific risks. By calculating conditional probabilities, we can anticipate complications like infection in patients with poor bone density or smoking habits, allowing for tailored risk reduction.
- Bayesian Updating (Wikipedia): Bayesian probability allows us to refine risk assessments based on new data, such as near misses or close calls. If a rare event nearly occurs in several cases, Bayesian updating can increase our perceived risk level and prompt adjustments to protocols.
- Failure Mode and Effects Analysis (FMEA) (Wikipedia): FMEA scores risk through three factors: severity, likelihood, and detectability. By multiplying these values, we prioritize high-severity, high-likelihood, and low-detectability risks, targeting specific mitigations for the highest risk scores.
- Poisson Distribution for Rare Events (Wikipedia): This statistical model can help predict the occurrence of rare events, like nerve damage or implant migration, over a larger sample of cases. It’s useful in planning for wild-type risks and justifies the need to monitor close calls.
By incorporating these mathematical approaches, dental professionals gain insights to enhance their risk management strategies, supporting better patient safety and clinical consistency.
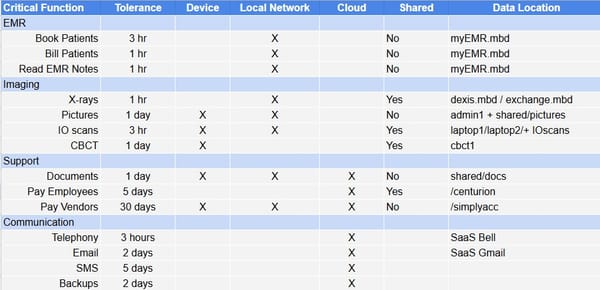
Integrating Risk Management into Protocols
A protocol-based approach ensures that risk management isn’t just case-specific but part of every interaction. This structure is essential for addressing frequent mild risks and preparing for wild-type events. A few key elements include:
- Standardized Preoperative Assessments: Comprehensive checklists streamline patient evaluations, identifying mild risks and potential red flags.
- Clear Communication: By setting clear expectations, we reduce misunderstandings and help patients understand why certain protocols, like follow-up visits, are essential.
- Close-Call Documentation: For wild-type risks, documenting close calls is crucial. Reviewing these events can help refine the protocol, potentially catching rare issues before they escalate.
These practices not only make risk management an integral part of our workflow but also support continuous improvement.
Evidence-Based Practice: Supporting Informed Choices
Risk management thrives on evidence-based practices. With thousands of implant systems available, selecting materials and techniques backed by research reduces variability and helps us make informed decisions. When addressing frequent, mild risks, meta-analysis, Cochrane reviews, and large-sample prospective studies offer actionable data, while for wild-type risks, evidence-based approaches help to focus on systems and practices with fewer rare complications.
For example, long-term studies show which systems perform well in high-risk scenarios. By consistently applying this knowledge, we provide patients with reliable, proven care.
Patient Communication: Setting Realistic Expectations
Risk management extends beyond clinical procedures to how we communicate with patients. Patients who understand the reasoning behind each decision are more likely to follow postoperative care and adhere to follow-up schedules, which is critical for managing both mild and wild-type risks.
When discussing risks, it’s important to be honest but reassuring. By explaining the proactive measures we’re taking, patients feel more informed and engaged in their care. A transparent approach builds trust and reinforces the importance of their role in achieving a successful outcome.
Continuous Learning and Adaptation
Effective risk management in dental implant surgery isn’t static; it’s an evolving process. Reviewing close calls and staying informed on research and best practices allow us to adapt and improve continuously. Each case contributes to a broader understanding of both predictable and unpredictable outcomes, guiding us toward lower risks and better results.
Strategic Risk Management for Consistent Success
In dental implant surgery, strategic risk management is about balancing rigorous planning with flexibility. By understanding mild and wild-type risks, adopting structured patient assessments, and embedding risk management into clinical protocols, we create a foundation for better patient care.
Ultimately, managing risk isn’t about avoiding every complication; it’s about adopting a systematic approach that prepares us to handle challenges confidently. This balance of preparation and adaptability allows us to navigate complex cases with precision and provide our patients with a high standard of care.