Deep Dive: Does Periodontitis Predict Implant Failure and Peri-Implantitis?

I often face a tough dilemma: when a patient has a failing tooth—or even an entire arch—due to severe periodontal issues, and I'm considering implants, I find myself wondering, "Just how high is the risk for peri-implantitis or implant failure in this case?"
Studies consistently show that a past of periodontal disease, particularly advanced periodontitis, is a strong predictor of complications with dental implants, including peri-implantitis and implant failure. But just how significant is this risk? Here, we’ll examine just how much periodontitis history influences implant outcomes and what we can do to help these high-risk patients beat the odds.
The Impact of Preexisting Periodontitis on Implant Outcomes
A strong connection exists between preexisting periodontitis and implant complications. Research shows that patients with a history of advanced periodontitis—referred to as periodontally compromised patients (PCP)—are at an increased risk of both implant loss and peri-implantitis. According to Roccuzzo et al. (2010), these patients experience significantly higher rates of implant failure and peri-implant bone loss than those with healthy periodontal histories, especially without regular supportive care (note that while I rely on the findings of Roccuzzo et al's work because it was a well-designed, long-term, prospective study, it still had a small sample size of 112).
The prevalence and rate of peri-implantitis among patients with a periodontitis history are substantial. Derks and Tomasi (2015a) found that peri-implantitis affects up to 22% (confidence interval: 14% to 30%) of implants in general, a considerable rate without additional risk factors. A second study from Derks et al (2015b) also investigated the impact of preexisting periodontitis on peri-implantitis rates in 11,391 implants. Researchers found that patients initially diagnosed with periodontitis had a higher odds ratio for early implant loss, which suggests an association between periodontitis and implant failure.
Furthermore, another study highlights that periodontally compromised patients often experience peri-implant bone loss at rates up to 30% faster than non-compromised patients (Roccuzzo et al., 2010). Once bone loss reaches 3 mm or more, implant failure rates spike to 15-20%, a steep increase from the typical 2-4% failure rate seen in healthier populations (Adler et al., 2019).
How Peri-Implantitis and Implant Failure Risk are Influenced by Patient History
Without regular maintenance, peri-implantitis progression accelerates significantly, particularly in patients with a history of severe gum disease. The dramatic variance in peri-implantitis rates, ranging from 1% to 47% across studies (Derks and Tomasi, 2015), largely underscores the impact of patient-specific factors like preexisting periodontitis, smoking, and diabetes. This variability is a clear indicator that, for PCP patients, risk mitigation needs to be as tailored as possible. It also supports the need for consistent preventive care for these high-risk patients.
Mitigating Risk for High-Risk Implant Patients
Given these elevated risks, evidence-based strategies are essential when treating patients with a history of periodontitis. Here’s what works:
- Regular Supportive Care as a Preventive Measure: Maintenance therapy, ideally every six months, is essential for high-risk patients. According to Roccuzzo et al. (2010), patients who adhered to a regular maintenance schedule showed about 1.5 mm less bone loss over ten years. This underscores that supportive care isn’t optional but rather critical to slowing peri-implantitis progression in periodontitis-affected patients.
- Thoughtful Patient Selection and Pre-Operative Planning: In patients who are not only periodontally compromised but also smokers or have poorly controlled diabetes, risk factors multiply. For instance, Adler et al. (2019) reported that smoking almost doubles the risk of peri-implantitis. For these patients, pre-operative cessation counseling, rigorous plaque control, and strategies like minimizing subgingival cement placement can significantly reduce implant failure risk.
- Loss of Bone: While the Derks et al (2015b) did not explicitly state that periodontitis directly causes early implant loss, it did point out that the consequences of periodontitis, such as advanced attachment and bone loss, lead to edentulous ridges with smaller dimensions which may necessitate the use of shorter implants (<10 mm). Therefore consideration to bone preservation, early extraction, or longer implants may have an indirect effect.
- Addressing Severe Cases with Implant Removal and Site Regeneration: When peri-implant bone loss becomes severe implant removal and site regeneration may be necessary. Though challenging, this approach allows for both functional and esthetic restoration. Cases that underwent re-implantation after site regeneration showed a 70% improvement in esthetic outcomes, particularly in areas with significant hard tissue loss (Wang et al., 2021).
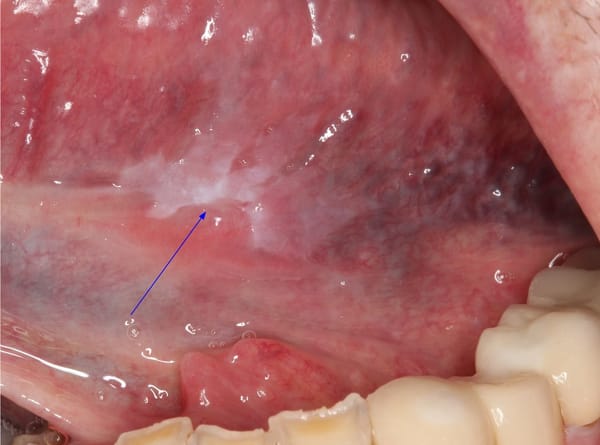
MRONJ and Peri-Implantitis: An Emerging Consideration
For patients on antiresorptive medications, the link between peri-implantitis and medication-related osteonecrosis of the jaw (MRONJ) is emerging as a critical risk factor. Derks and Tomasi (2015) suggest that patients with peri-implantitis and a history of bisphosphonate use may be at increased risk for MRONJ. For clinicians, monitoring peri-implant health and educating patients about MRONJ risks are crucial in high-risk, periodontally compromised patients on these medications.
Toward a Personalized Approach
The data makes it clear: regular maintenance, patient-specific risk assessment, and customized surgical planning are essential to managing implants in patients with a history of periodontitis. By focusing on individualized care, we’re not just addressing peri-implantitis risk; we’re working toward stable, long-term outcomes for every patient.